A Few Simple Guidelines
Sometimes, teeth need to be removed due to decay, disease or trauma. Having a tooth removed or “pulled” is called a tooth extraction.
When you have an extraction, it’s natural that changes will occur in your mouth afterward. Your dentist may give you instructions to follow after the extraction, and it’s important to talk to your dentist if you have any questions or problems. Here are some general guidelines to help promote healing, prevent complications, and make you more comfortable.
Anesthetics
Before the extraction, you will be given an anesthetic to reduce your discomfort. Your mouth will remain numb for a few hours after the extraction. While your mouth is numb, you’ll want to be careful not to bite your cheek, lip or tongue. After the extraction, do not eat any foods that require chewing while your mouth is numb. The numbness should go away within a few hours. If it doesn’t, contact your dentist.
Bleeding
Your dentist may place a gauze pack on the extraction site to limit bleeding. This will also help a blood clot to form, which is necessary for normal healing. This gauze pack should be left in place for 30 to 45 minutes after you leave the dentist’s office. Do not chew on the pack. There may be some bleeding or oozing after the pack is removed. If so, here’s what to do:
- Fold a piece of clean gauze into a pad thick enough to bite on. Dampen the pad with clean, warm water and place it directly on the extraction site.
- Apply pressure by closing the teeth firmly over the pad. Maintain this pressure for about 30 minutes. If the pad becomes soaked with blood, replace it with a clean one.
- Do not suck on the extraction site or disturb it with your tongue.
- A slight amount of blood may leak from the extraction site until a clot forms. However, if heavy bleeding continues, call your dentist. (Remember, though, that a little bit of blood mixed with saliva can look like a lot of bleeding.)
Do Not Disturb!
The blood clot that forms in the tooth socket is an important part of the normal healing process. You should avoid doing things that might disturb the clot. Here’s how to protect it:
- Do not rinse your mouth vigorously, or drink through a straw for 24 hours. These activities create suction in the mouth, which could loosen the clot and delay healing.
- Avoid alcoholic beverages or mouthwash containing alcohol for 24 hours.
- If you are a smoker, talk to your dentist before the surgery on ways to quit. You should not smoke after surgery.
- Limit strenuous activity for 24 hours after the extraction. This will reduce bleeding and help the blood clot to form.
- Sometimes the blood clot does not form in the first day or two after the extraction, or it forms but breaks down. The result is called dry socket. This can be very painful and should be reported to your dentist. A dressing may be placed in the socket to protect it until the socket heals and to reduce any pain.
Cleaning Your Mouth
Do not clean the teeth next to the healing tooth socket for the rest of the day. You should, however, brush and floss your other teeth well and begin cleaning the teeth next to the healing tooth socket the next day. You can also brush your tongue. This will help get rid of the bad breath and unpleasant taste that are common after an extraction.
The day after the extraction, gently rinse your mouth with warm salt water (half a teaspoon salt in an 8 oz. glass of warm water) after meals to keep food particles out of the extraction site. Try not to rinse your mouth vigorously, as this may loosen the blood clot. If you have hypertension, discuss with your dentist whether you should rinse with salt water. Avoid using a mouthwash during this early healing period unless your dentist advises you to do so.
Medication
If your dentist has prescribed medicine to control pain and inflammation, or to prevent infection, use it only as directed. If the pain medication prescribed does not seem to work for you, do not take more pills or take them more often than directed—call your dentist.
Swelling and Pain
After a tooth is removed, you may have some discomfort and notice some swelling. This is normal. To help reduce swelling and pain, try applying an ice bag or cold, moist cloth to your face. Your dentist may give you specific instructions on how long and how often to use a cold compress.
When to Call the Dentist
- fever, nausea or vomiting
- ongoing or severe pain, swelling, or bleeding
- pain that gets worse with time instead of better
If you have any of the following issues, call your dentist immediately. If you cannot reach your dentist, go to a hospital emergency room.
Eating and Drinking
Eating & Drinking After a Tooth Extraction After the extraction, drink lots of liquids and eat soft, nutritious foods. Avoid hot liquids and alcoholic beverages. Do not use a straw. Begin eating solid foods the next day or as soon as you can chew comfortably. For the first few days, try to chew food on the side opposite the extraction site. When it feels comfortable, you should resume chewing on both sides of your mouth.
Follow-Up
If you have sutures that require removal, your dentist will tell you when to return to the office.









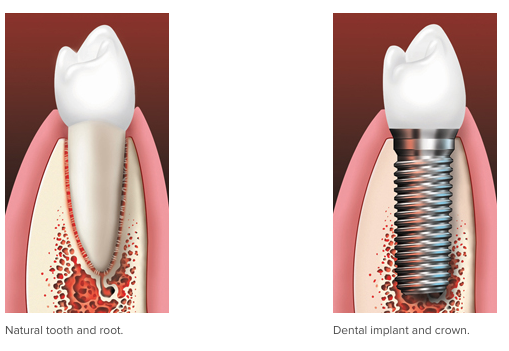
 Complete Dentures: Complete dentures are made of a plastic base that is colored in order to replicate gum tissue and supports a full set of plastic or porcelain teeth. The traditional full denture is held in the mouth by forming a seal with the gums. They can also be held in place by attaching to dental implants that are surgically placed in the bone of the jaws. This treatment is much more expensive than the traditional complete denture.
Complete Dentures: Complete dentures are made of a plastic base that is colored in order to replicate gum tissue and supports a full set of plastic or porcelain teeth. The traditional full denture is held in the mouth by forming a seal with the gums. They can also be held in place by attaching to dental implants that are surgically placed in the bone of the jaws. This treatment is much more expensive than the traditional complete denture.